ASCORAD: The Next-Generation Atopic Dermatitis automatic scoring system
Introduction
Legit.Health proudly introduces a significant advancement in dermatological assessments: the ASCORAD (Automatic SCORing Atopic Dermatitis) system. This innovative tool leverages advanced computer vision algorithms to analyze images captured by smartphones and automatically align them with the SCORAD scoring system.
The ASCORAD has been recognized and validated in multiple scientific publications. A comprehensive systematic review published in Artificial Intelligence in Medicine highlights ASCORAD's superior performance:
(...) very promising is the attempt to arrive at an automatic definition of AD severity by using CNNs (...) to achieve a scoring accuracy of erythema, papulation, excoriation, and lichenification severity comparable to that of dermatologists (...). Computational applicative advances in this direction have led to the more recent design of Automatic SCORing Atopic Dermatitis (ASCORAD).
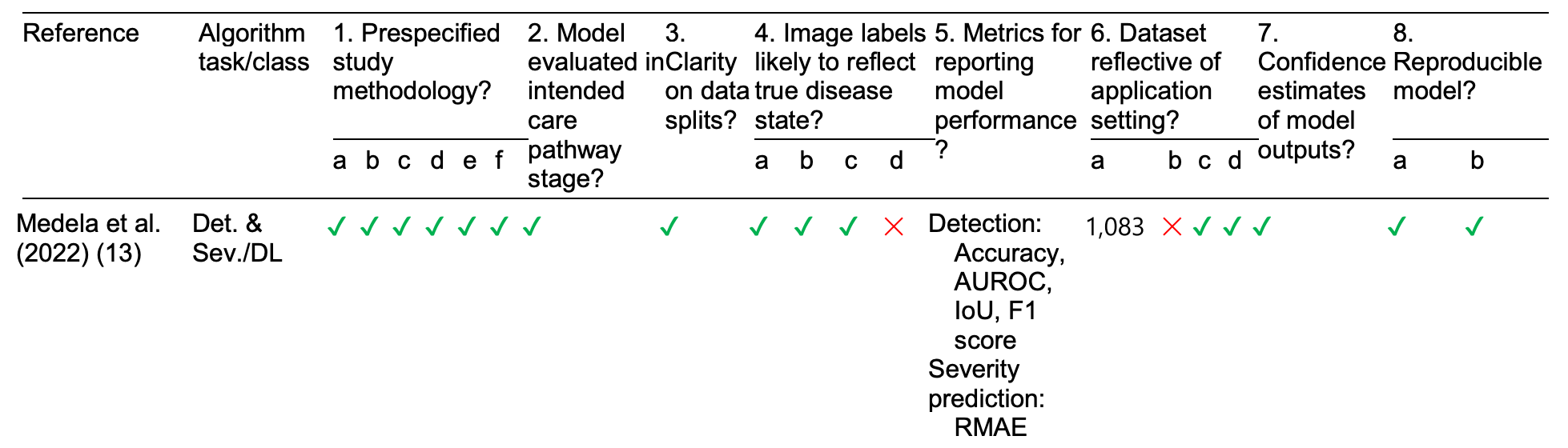
Furthermore, in a comprehensive systematic review published in Artificial Intelligence in Medicine analyzing AI-powered tools for eczema assessment, ASCORAD stands out among all evaluated systems and demonstrated superior performance metrics, being one of the few solutions that successfully combines both eczema area detection and severity prediction in an integrated approach.:
Overview of the quality of existing AI-powered eczema area detection and severity prediction studies.
Indeed, objective, reliable, and precise measurement tools are foundational to evidence-based healthcare. The integration of ASCORAD into Legit.Health's suite of tools represents a paradigm shift in how atopic dermatitis is evaluated and managed. By automating the SCORAD process, ASCORAD not only enhances the accuracy and reliability of assessments but also streamlines the workflow for healthcare professionals, setting a new standard for dermatological care.
Do you want to see the clinical AI technology in action?
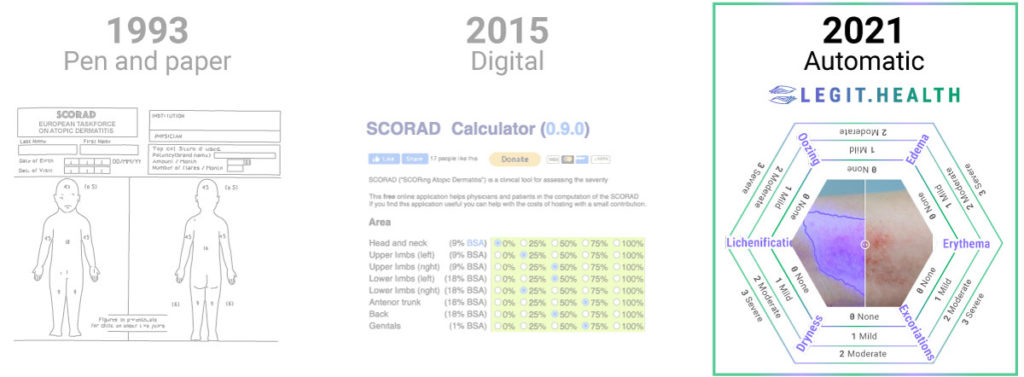
A lot has changed since 1993
We owe a lot to the European Task Force on atopic dermatitis that published the first SCORAD paper in 1993. They were trying to tackle a huge obstacle both in clinical practice and clinical trials. As the authors stated:
Assessment methods for atopic dermatitis (AD) are not standardized, and therapeutic studies are difficult to interpret.
This was the premise that led renown professors Alain Taïeb and Jean-François Stalder to take on the difficult task of developing a composite severity index along with a brilliant team of researchers. The creation of the SCORAD was a stroke of genious and a huge contribution to the medical knowledge of human civilisation.
The pen and paper SCORAD
The solution proposed in 1993 may seem somewhat old school today, but it is a very bright way of tackling the problem. They aimed to create an evaluation system that excelled in simplicity and ease of use. To do so, they created the following sheet of paper:
Sheet of paper containing the SCORAD template for clinical practice.
The SCORAD Index formula is: A/5 + 7B/2 + C. In this formula, A is defined as the extent (0-100), B is defined as the intensity (0-18) and C is defined as the subjective symptoms (0-20). The maximum score of the SCORAD Index is 103.
Watch this video where one of the creators of the SCORAD, professor Jean-François Stalder, interacts with one of the creators of the ASCORAD, Taig Mac Carthy. Clips extracted from the event "Artificial intelligence: what future for eczema patients?"
organised by the Pierre Fabre Eczema Foundation on Sep 14th 2023
Despite the widespread acceptance and utility of the SCORAD and EASI in atopic dermatitis evaluation, there is a notable caveat associated with these tools:
Indeed, the SCORAD scoring system is representative and well evaluated, but shows, as with all other systems, intra and interobserver disagreements. The variation in scores is about 20%.
The digital approach: online calculators
With the digital revolution and the rise of computers, researchers from all over the world developed digital versions of the pen-and-paper SCORAD.
The main advantage of these systems is that they automatically perform the calculation of the formula A/5 + 7B/2 + C, and that's why people call them digital calculators. However, digital calculators have the same limitations as their pen-and-paper precursors: they are still very subjective and require a lot of time, as well as knowledge, to properly use them.
Having to estimate the redness or the desquamation of the affected area with the naked eye, just by looking at, it feels very outdated.
The next generation: automatic scoring
Legit.Health is the revolutionary clinical data and communication tool for next-generation dermatologists that triples the reliability of outcome measures. The technology speeds up the pathology reporting process and increases patients' autonomy and control.
This means that the new version of this scoring system extracts data precisely and consistently, both during routine evaluations and clinical research. The improvement can be seen in the following table, which compares the performance metrics of the most common way of using scoring systems:
| Pen and Paper | Digital | Automatic (AI) | |
|---|---|---|---|
| Self-supervision | - | - | Perform diagnosis |
| Ease of use | ≈ 600 seconds | ≈ 420 seconds | ≈ 23 seconds |
| Sensitivity to change | 0 to 4 | 0 to 4 | 0 to 100 |
| Interobserver variability | Medium (20%) | Medium (20%) | Lowest (8%) |
| Intra-observer variability | High | High | Zero |
Table 1: comparison between different methods of scoring the severity of a disease. The automatic artificial intelligence-powered method performs better across most performance indicators.
Thanks to the deep learning algorithms, Legit.Health relieves doctors from the tedious manual calculation of scoring systems and allows the practice of a more objective evidence-based dermatology. Also, by using algorithms to measure dryness, lichenification, erythema, oozing, oedema, and many more signs, the tool can calculate visual signs in a more reliably and consistently.
Do you want to see the clinical AI technology in action?
The problem with the SCORAD
It is a well-documented fact that SCORAD is a valid, internally consistent, responsive, interpretable composite score that includes the intensity and extent of clinical signs of atopic dermatitis and the severity of its symptoms
That is precisely why Legit.Health has chosen this scoring system to serve as the basis for its revolutionary algorithm. In other words: the SCORAD becomes the framework to automate the scoring of the disease with deep learning. However, the traditional SCORAD carries a set of problems and limitations
Scoring systems like SCORAD and EASI have an inter-observer variability and are time consuming. An AI automated approach like ours may help to reduce such bias and therefore be a more precise and objective criterion
As well as that, filling up the sheet has proven to be too tedious for some dermatologists. In many cases, doctors deem that the effort of filling in the SCORAD is too high and they end up not using it in their day-to-day clinical practice. This may be the main reason behind the popularity of the EASI, which sacrifices granularity for the benefit of becoming a simpler and quicker scoring system.
ASCORAD improves the clinimetric properties of SCORAD and becomes a better outcome measure.
How do we know if a scoring system is good?
When it comes to dermatological assessments, the effectiveness of a scoring system is paramount. But what exactly makes a scoring system reliable and useful? Through scientific consensus, several key factors have been identified that contribute to the robustness of these systems. Let's delve into these crucial elements:
- Ease of Use: This factor considers whether the system can be applied effortlessly within the constraints of time and financial resources. A user-friendly system is crucial for widespread adoption in clinical settings.
- Sensitivity to Change: An effective scoring system must be capable of detecting clinically meaningful changes over time. This sensitivity ensures that any progress or deterioration in a patient's condition is accurately captured.
- Interobserver Reliability: This refers to the consistency of the results when different observers use the scoring system. High interobserver reliability means different clinicians will arrive at similar conclusions, enhancing the system's credibility.
- Intra-observer Variability: This looks at the consistency of results when the same observer uses the scoring system multiple times. Low intra-observer variability indicates that the system provides stable results, irrespective of repeated assessments by the same clinician.
- Interpretability: A practical scoring system should provide meaningful qualitative interpretations of its scores, like categorizing the severity of a condition as mild, moderate, or severe.
These criteria not only ensure the scoring system's effectiveness but also its applicability and reliability in diverse clinical scenarios.
Adapted from "Methods and definitions to rate the quality of outcome measures". Schmitt, J., Langan, S., Deckert, S., Svensson, A., von Kobyletzki, L., Thomas, K., & Spuls, P. (2013). Assessment of clinical signs of atopic dermatitis: A systematic review and recommendation. Journal of Allergy and Clinical Immunology, 132(6), 1337--1347. doi:10.1016/j.jaci.2013.07.008.
6 ways in which ASCORAD enhances atopic dermatitis diagnosis
ASCORAD is defined as:
(...) a fast and objective alternative method for the automatic assessment of atopic dermatitis with great potential, already achieving results comparable to human expert assessment, whilst greatly reducing inter-observer variability and being more time-efficient. ASCORAD could also be used in situations where face-to-face consultations are not possible, providing an automatic assessment of clinical signs and lesion surface.
Legit.Health's algorithms automatically grade lesions just by looking at smartphone images and small patient-reported outcome measures (PROMs). In other words: the tool will automatically fill in most of the dermatology scoring systems, such as PASI, SCORAD, UAS, GAGS, and many more.
The main goal of ASCORAD is to provide a tool to record data precisely and consistently for routine evaluations and clinical studies.
1. It's self supervised: the algorithm makes sure it's atopic dermatitis
When using the ASCORAD, medical professionals are assessing the diagnosis of the pathology while estimating the severity. This means that if the ASCORAD is the wrong scoring system because it's not really atopic dermatitis, the tool with let the doctor know that there may be a mismatch.
Legit.Health's tool not only measures the severity of the affection as the SCORAD does but the algorithm has been trained using the input of top doctors in their field to be able to distinguish between hundreds of conditions, most kinds of dermatitis included.
This means that ASCORAD will not confuse a case of atopic dermatitis with some of the usual suspects for misdiagnosis such ass neurodermatitis or sebaceous dermatitis, improving the rate of correct diagnosis of the doctor by 23%
2. ASCORAD is easier to use than SCORAD and EASI
The [traditional] SCORAD system takes time and even experienced dermatologists will require seven (7) minuntes in total. An inexperienced physician will need 10 minutes.
In comparison, using the ASCORAD only takes 23 seconds to get the final score, and most of that time is consumed in taking the picture. Additionally, said score and the image it came from are neatly archived and labelled for future assessment.
ASCORAD estimates the affected surface and the intensity of all visual signs of the disease simultaneously, improving the efficiency of both tasks.
Do you want to see the clinical AI technology in action?
Overall, ASCORAD helps practice evidence-based dermatology, relieving doctors from the tedious SCORAD calculation, enabling patients to track atopic dermatitis severity in a user-friendly and objective way, and allowing a more precise evaluation of new treatments.
3. ASCORAD has the highest sensitivity to change
Legit.Health's tool identifies pathologies using validated score systems that have:
- Lowest Minimal Important Difference (MID)
- Lowest Smallest detectable Change (SDC)
- Higher validity and reliability
Furthermore, the algorithms provide additional data with comparable clinimetric properties and higher sensitivity to change and MIDs, thanks to the intrinsic functioning of computer vision algorithms.
4. Lowest inter-observer variability
Indeed, the SCORAD scoring system is representative and well evaluated, but shows, as with all other systems, intra and interobserver disagreements. The variation in scores is about 20%.
The experimental results show that ASCORAD can achieve the mean absolute percentage error of 8%, outperforming baseline methods and below the inter-observer variability of 20%.
5. Zero intra-observer variability
The digital nature of the ASCORAD system eliminates completely the intra-observer variability, as every image and calculation is stored in the app's database.
Allowing the doctor to not rely on his memory when assessing the severity of the affection and focusing on the analysis of the objective data stored in the app reduces considerably the risk of misremembering, providing a more objective, accurate, and precise way of tracing the development of the disease.
6. Better interpretability
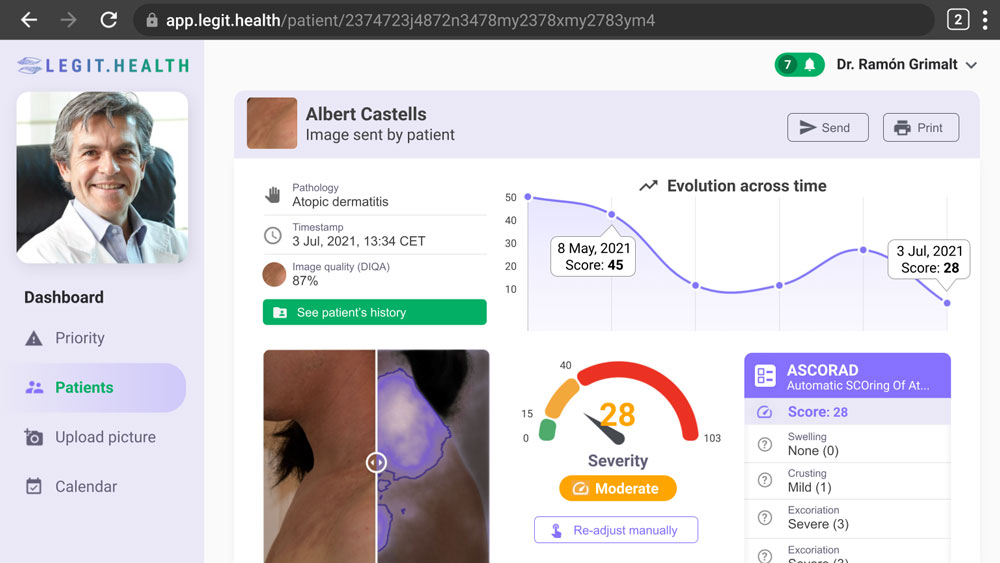
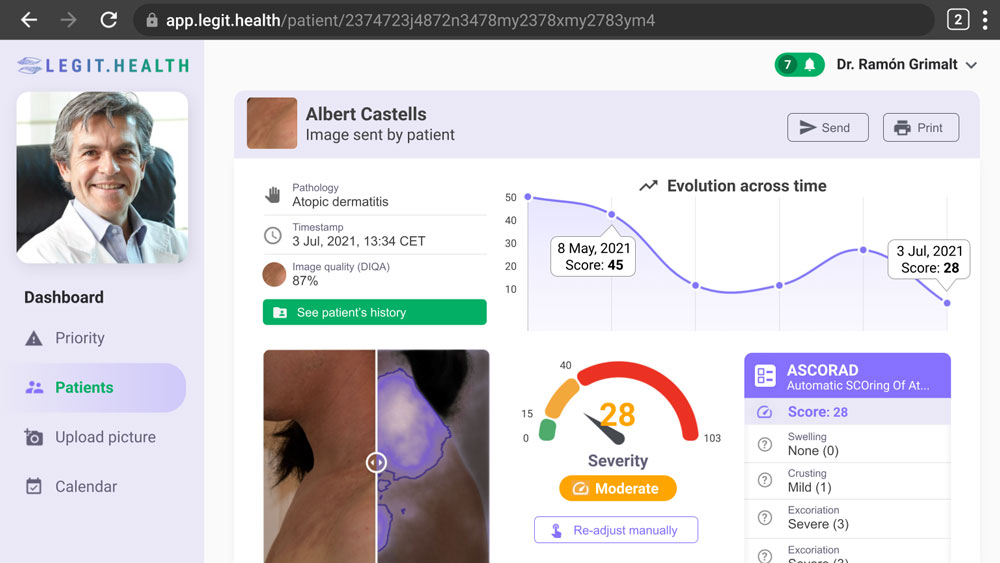
Legit.Health provides an easy-to-read interface that gives the doctor access to all the relevant information about the patient in one look.
Every data derived from the ASCORAD is displayed clearly on the screen, providing the severity of the affection, the different factors considered when analyzing the image and their punctuations, and an evolution across time graff that follows the healing process effectiveness of the treatment really easily.
Additionally, every photo of the patient's history is easily accessible, providing a backlog of images where the algorithm highlights the affected areas automatically.
In conclusion
The revolutionary ASCORAD represents the future of dermatology. Allowing doctors across the globe to practice evidence-based medicine by using the best tool during the disease diagnosis while improving the effective communication between doctor and patient.
The use of algorithms that estimate the severity of atopic dermatitis by filling up the SCORAD and automatically score lesions just by looking at smartphone images increases the doctors' correct diagnosis rate by 23% and improves the following of the treatment by making the patient a more active participant on its own recovery.
Get access now
Get started
AI-powered dermatology validated by peer-reviewed research. Trusted by leading hospitals across Europe. Fill in the form to see how our CE-marked platform can transform your practice.