APASI: The bright future of Psoriasis severity assessment has arrived
Introduction
The future of dermatology has arrived thanks to Legit.Health's revolutionary application of the PASI system: APASI (Automatic Psoriasis Area and Severity Index). Using computer vision algorithms, the researchers have created a tool that processes smartphone images and automatically translates them into the domain of the PASI.
It is widely known that objective, reliable, and precise outcome measures are key to evidence-based medicine. When considering psoriasis, the PASI has the best measurement properties and is the most recommended for clinical trials. That is why we automated the PASI to help patients and doctors achieve better health outcomes.
The origins of the PASI
This scoring system for psoriasis was first published in a paper by T. Fredericksson and U. Pettersson in 1978, where they explored the validity of a new treatment for the disease.
Their formula for assessing the severity of the condition would go on to become the gold standard for dermatologists around the globe and is still widely used to this day.
In order to calculate the PASI, the sum of the severity of these three main changes was multiplied with the numerical value of the areas involved and with the various percentages of the four body areas. These values were then added in order to obtain the PASI.
PASI score sheet by British Columbia Ministry of Health
The shortfalls of the pen-and-paper PASI
The main goal of PASI is to provide a tool to record data precisely and consistently for routine evaluations and clinical studies. However, it carries a set of problems and limitations.
We found substantial variation [in the results] between experienced and inexperienced physicians using PASI
In other words, there is a high inter-observer variability, that is most pronounced when compared between experienced and inexperienced practitioners.
Aside from the inter-observer variation, many physicians have reported that filling up the paper sheet is too tedious and time-consuming and that they don't really use it on a day-to-day basis.
Do you want to see the clinical AI technology in action?
Digital calculators: A half-baked solution to the problem
With the advent of basic computation, several digitalized versions of the PASI scoring system were developed, in an attempt to reduce the time wasted in calculations. These online calculators tackle, although inefficiently, just one of the issues the traditional PASI has. While the formula is calculated automatically, the doctor still has to fill in the value for each parameter.
This not only still requires the time and attention of the physician, but does nothing to address the multiple issues of lack of objectivity and reproducibility within the PASI system.
How do we know if a scoring system is good?
When it comes to dermatological assessments, the effectiveness of a scoring system is paramount. But what exactly makes a scoring system reliable and useful? Through scientific consensus, several key factors have been identified that contribute to the robustness of these systems. Let's delve into these crucial elements:
- Ease of Use: This factor considers whether the system can be applied effortlessly within the constraints of time and financial resources. A user-friendly system is crucial for widespread adoption in clinical settings.
- Sensitivity to Change: An effective scoring system must be capable of detecting clinically meaningful changes over time. This sensitivity ensures that any progress or deterioration in a patient's condition is accurately captured.
- Interobserver Reliability: This refers to the consistency of the results when different observers use the scoring system. High interobserver reliability means different clinicians will arrive at similar conclusions, enhancing the system's credibility.
- Intra-observer Variability: This looks at the consistency of results when the same observer uses the scoring system multiple times. Low intra-observer variability indicates that the system provides stable results, irrespective of repeated assessments by the same clinician.
- Interpretability: A practical scoring system should provide meaningful qualitative interpretations of its scores, like categorizing the severity of a condition as mild, moderate, or severe.
These criteria not only ensure the scoring system's effectiveness but also its applicability and reliability in diverse clinical scenarios.
Adapted from "Methods and definitions to rate the quality of outcome measures". Schmitt, J., Langan, S., Deckert, S., Svensson, A., von Kobyletzki, L., Thomas, K., & Spuls, P. (2013). Assessment of clinical signs of atopic dermatitis: A systematic review and recommendation. Journal of Allergy and Clinical Immunology, 132(6), 1337--1347. doi:10.1016/j.jaci.2013.07.008.
Six ways in which APASI is better
Legit.Health is the revolutionary Clinical Data and Communication tool for Next-generation dermatologists that triples the empowerment of patients.
After 12 months using Legit.Health, in which we analysed the applicability of the tool at our hospital, we have drawn conclusions that help to propose a new care paradigm in the follow-up of psoriasis.
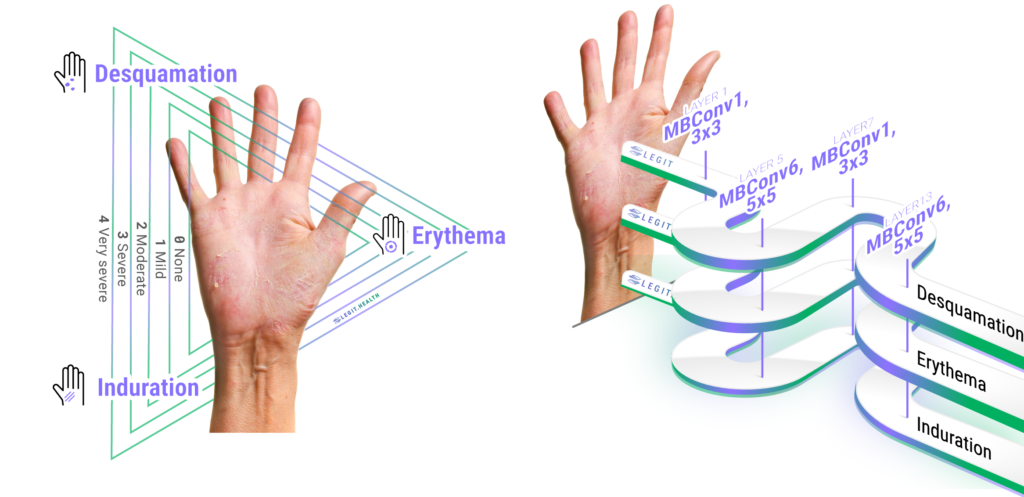
The purpose of the deep learning algorithms is to relieve doctors from the tedious manual calculation of scoring systems and allow the practice of more objective evidence-based dermatology while speeding up the pathology reporting process and increasing patients' autonomy and control.
Legit.Health's algorithms automatically grade lesions just by looking at smartphone images and small patient-reported outcome measures (PROMs). In other words: the tool will automatically fill in most of the dermatology scoring systems, such as PASI, SCORAD, UAS, GAGS, and many more.
This means that the new version of this scoring system extracts data precisely and consistently, both during routine evaluations and clinical research. The improvement can be seen in the following table, which compares the performance metrics of the most common way of using scoring systems:
| Pen and Paper | Digital | Automatic (AI) | |
|---|---|---|---|
| Self-supervision | - | - | Perform diagnosis |
| Ease of use | ≈ 600 seconds | ≈ 420 seconds | ≈ 23 seconds |
| Sensitivity to change | 0 to 4 | 0 to 4 | 0 to 100 |
| Interobserver variability | Medium (20%) | Medium (20%) | Lowest (8%) |
| Intra-observer variability | High | High | Zero |
Table 1: comparison between different methods of scoring the severity of a disease. The automatic artificial intelligence-powered method performs better across most performance indicators.
Thanks to the deep learning algorithms, Legit.Health relieves doctors from the tedious manual calculation of scoring systems and allows the practice of a more objective evidence-based dermatology. Also, by using algorithms to measure dryness, lichenification, erythema, oozing, oedema, and many more signs, the tool can calculate visual signs in a more reliably and consistently.
1. Easier to use and faster than any other existing method
While an experienced physician might take six to seven minutes to completely fill in and calculate the PASI score of a patient, an inexperienced one will need ten minutes. Meanwhile, Legit.Health's algorithm only takes 23 seconds to get the final score, including capturing the image.
This is key both from a time management perspective, allowing the doctors better use their time with the patient, and from a clinical perspective. The fact that many physicians won't fill in any scoring system for considering the process too tedious and time-consuming and would rather make a gut estimate of the severity of the disease is incompatible with the modern idea of practising evidence-based medicine.
2. APASI assists the doctor in the diagnosis of the disease
The algorithm developed by Legit.Health isn't limited to simply measuring the severity, like the PASI does. It can also help assess whether or not the condition is actually psoriasis. The APASI has been trained using the input of top dermatologists to distinguish between hundreds of conditions, including most types of psoriasis.
This means that APASI will distinguish between several types of psoriasis and assist the doctor in the disease assessment process, not only making it quicker by providing relevant information but improving the rate of correct diagnosis by 23%
Do you want to see the clinical AI technology in action?
3. APASI can detect small changes in the evolution of the pathology
Legit.Health's tool analyzes the pathologies using a validated scoring system that has both the lowest MID (Minimal important Difference) and is sensible to the lowest LDC (Lowest Detectable Change), which means the algorithm analyzes every image with more precision and attention to detail than any human observer would.
In clinical trials, quantification of the disease is critical to measure the efficacy of an investigational treatment by comparing the severity of disease before therapy to that measured after treatment.
Furthermore, it has a higher validity and reliability while maintaining comparable clinimetric properties, thanks to the intrinsic functioning of computer vision algorithms.
4. Greatly reduces inter-observer variability
Our data indicate that even experienced investigators had difficulty with PASI in rating the area of involvement […], especially among patients with more severe psoriasis.
The experimental results show that APASI outperforms the baseline methods when it comes to inter-observer variability, achieving a mean absolute percentage of error of just 13%, way below the usual 20% that can be observed in the classical application of the traditional scoring systems.
5. Zero intra-observer variability
The algorithmic nature of the APASI eliminates entirely, and without question, the intra-observer variability, as every reading is reliably consistent.
This allows the doctor to not rely on his memory when assessing the severity of the psoriasis, so they can focus on the analysis of the contextual information. In this sense, the more objective data reduces considerably the risk of misdiagnosing, providing a more objective, accurate, and precise way of tracing the development of the disease.
To judge a treatment effect, the variation in rating a patient from time to time should be low
This becomes especially important in clinical trials, where reducing this kind of variability is key to gathering the precise data required in this kind of study.
6. More accessible and easier-to-read data
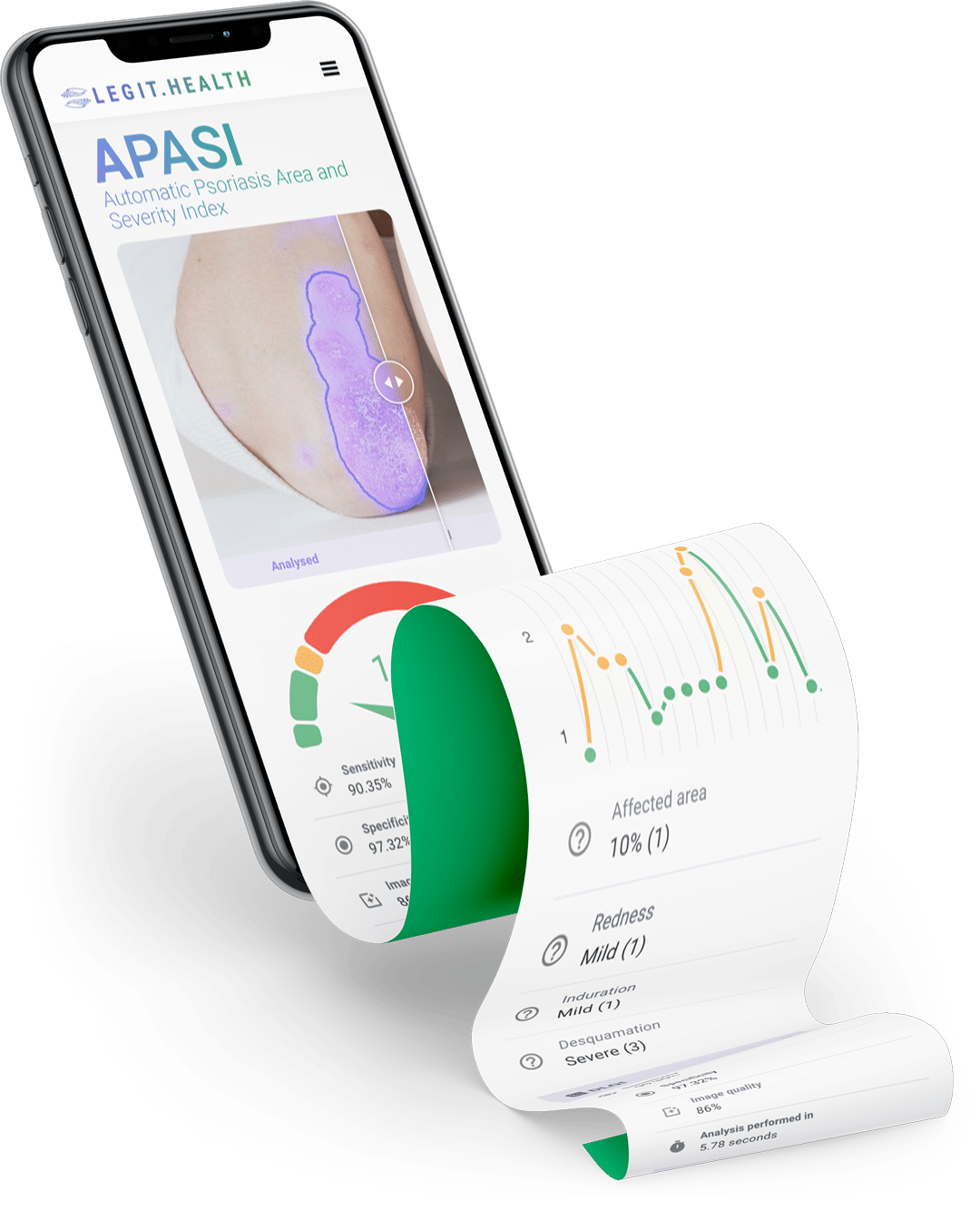
Last but not least, Legit.Health's interface provides access to all the relevant information about the patient in an easy-to-read manner.
Every data derived from the APASI is clearly displayed on the screen, showing the severity of the affection and the different factors considered by the algorithm when analyzing the image and their scores.
The app also provides a handy graff that shows the evolution of the disease across time and makes following the healing process and the effectiveness of the treatment really easy.
Do you want to see the clinical AI technology in action?
In conclusion
The revolutionary and innovative APASI represents the future of dermatology. We are giving doctors access to the best tool for the diagnosis of psoriasis and allowing them to practice evidence-based medicine and improve the communication between doctor and patient.
Thanks to Legit.Health, doctors across the globe can improve their correct diagnosis rate by 23% and make treatment easier to follow for the patient by making them active participants in their own recovery.
There is no denying that the use of algorithms that estimate the severity of the disease represents a bright future for the practice of dermatology and that will, without doubt, help advance the field.
Get access now
This free 23-day trial of Legit.Health gives clinics and hospitals a hands-on look at how to drive increased adherence and improve patient outcomes, as well as improving efficiency and overall quality of life.

